Guide to the COVID-19 Pandemic
Key Points
- Check your local COVID dashboard and know your local situation.
- If you’re in an area where case numbers are low and/or declining, please remember to continue to practice basic precautions until your country has eliminated the virus or until we have a vaccine.
- If you’re in an area with high or increasing case numbers your personal precautions will be even more important, but are also highly effective.
- Remember that people can transmit the virus without being visibly sick.
- Don’t panic, remember that what you do makes a difference. Your actions can protect yourself, your family and your community.
Activity Risk Guide
Note: If in an area with high or increasing virus transmission it is best to avoid all high and medium risk activities, but as your community controls the outbreak, it is acceptable to slowly phase in medium risk activities. Only when your community has stopped viral transmission is it safe to phase in some more high risk activities (though continue to take the core precautions outlined above (hand washing, wear a face covering, don’t touch your face, practice physical distancing, stay at home if sick). These activities are largely based on recent research that has identified the activities that are most likely to result in disease transmission.
High Risk Activities (avoid unless essential)
- Don’t eat at indoor restaurants (this has been highlighted in recent research as one of the most risky activities).
- Don’t go to indoor fitness centers.
- Don’t eat or work at indoor cafes.
- Don’t travel unless you have to for medical or other essential reasons, and if travelling try to avoid staying at a hotel. If you do have to stay, choose a hotel with an outside entrance to the room, instead of having to walk through a lobby.
- If attending a religious service, choose one being held outdoors. If attending indoors, ensure the organization has limited the number of people that can be inside at one time, has made accommodations for physical distancing, requires face coverings and avoids singing.
- Don’t go to any indoor public spaces, don’t have friends over or go to others’ homes (except for people that you have formed a pod with).
- Don’t have regular services come to your house (e.g. cleaners), unless necessary.
- Don’t go to the doctor or hospital unless it is urgent, call first.
- Don’t simply believe what you read on social media, confirm it on trusted sites.

Medium-Low Risk Activities (reduce and use precautions, see FAQ below)
- Getting takeout food.
- Getting packages delivered to your door (not inside the house).
- Going for walks or exercising outside (keeping 6 feet of separation from others).
- Taking public transportation, taxis or Ubers (keeping distance from others when possible).
- Going to the store for food and supplies.
Beneficial Activities
- Take care of yourself, eat well, exercise, get a good night’s sleep
- Wash your hands regularly and keep your house clean.
- Prepare in case you have to isolate for two weeks.
- Practice good financial planning and management.
- Stay in touch with others and help your community.
The Situation and Key Updates (as of 6 June 2021):
- We are in the middle of a coronavirus pandemic that started in Wuhan China in December 2019.
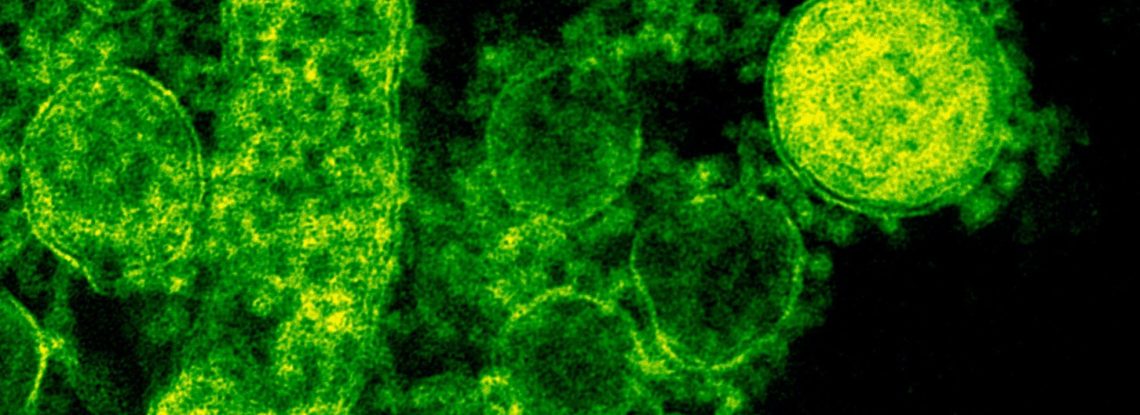
- The virus is called SARS-CoV-2 and the disease is called COVID-19.
- There are over 174 million cases worldwide that have resulted in over 3,700,000 deaths.
- Internationally, there is highly variable vaccine rollout, with some countries nearing 50% fully vaccinated, while other are at 5% or below.
- Despite this high number of cases and vaccinations, we are nowhere near the level needed to achieve herd immunity (where enough of the population is immune to a disease to stop its spread). We don’t know if herd immunity is possible for COVID-19 and even if herd immunity is achievable for COVID-19, we would need 70+% of the population to be immune.
- The US is remains the center of the pandemic, with over 34 million cases and 612,000 fatalities, though India currently has the highest number of new daily cases at nearly 115,000 per day.
- While vaccination and restrictions have slowed viral transmission in many countries, new more-transmissible and somewhat vaccine-evading variants have combined with a relaxing of restrictions leading to increasing case numbers in several countries, such as the UK.
- Unfortunately the pandemic is also increasing many existing health inequities in the US and other countries. To understand more about this issues, please see this analysis from the British Medical Journal.
- The highest number of cases right now is in the under 30 age group. While young adults and children are at a lower risk of death from COVID-19 they are still at a high risk of serious or long-term illness (i.e. Long COVID) and can contribute to transmission of the virus throughout the community.
- It is thought that 20% or more of COVID-19 cases result in persistent symptoms that do not resolve even after the body has eliminated the virus. We often see these serious and persistent symptoms in health young adults that had ‘mild’ COVID-19 cases. We are all at risk of long-COVID and all ages need to be exercising precautions.
- We are discovering that children and schools may pose more of a risk of virus transmission than we had previously thought, especially with the new variants. In-person learning is critical but also needs to be approached with caution. In areas with low virus transmission schools can typically open with low-medium risk (provided they use upgraded cleaning, require face coverings and preferable perform routine testing). However, the safest way to reopen schools is for the community to first eliminate virus transmission (this is still possible).
- Most virus transmission occurs before, or just as people exhibit symptoms. Because of this, it is vital to wear face coverings when in public. Face coverings will not prevent you from getting the virus but they will reduce the possibility of you spreading the virus to others. Remember that you can spread the virus before you know you’re sick and infected. Face coverings have been shown to be very effective in reducing transmission in communities, especially when everyone participates. Despite the recent CDC guidance, it is still recommend to wear face coverings when in public, even if you are vaccinated. This is because the vaccines do not provide perfect protection and it is still possible for vaccinated people to spread the virus (though at a significantly reduced level).
- Containing this pandemic is only possible if each of us act to protect ourselves, our family, our neighbors and our communities. Our individual actions ARE making a difference.
The Disease:
- Most COVID-19 cases are mild flu-like respiratory infections, causing aches, fever and coughing. Some people also experience: sore throat, vomiting, diarrhea, rash, conjunctivitis or changes in smell or taste. Changes in smell or taste are often the first symptoms that develop.
- On average, it takes 5 days from when you are infected till you develop symptoms, these symptoms then increase over time and typically last for 8 days. You are most likely to spread the virus during the first week of infection (including before you show most symptoms). You may still test positive for the virus even after your symptoms resolve, but the risk of spreading the virus is low at that point.
- About 10-20% of the cases develop pneumonia that may require hospitalization. Those at high-risk of this occurring include those over 70 and those with other serious health conditions, including: cardiovascular disease, hypertension, diabetes, respiratory disease, cancer, anyone taking immuno-suppressant therapies (e.g. steroids or others) and anyone that smokes or is overweight. In addition, men seem to be at twice the risk of serious infection. If any of these risks applies to you, be extra cautious.
- In some cases the virus can cause a wide range of symptoms that range from blood clotting disorders to neurological issues. In some cases these symptoms persist even after the body has eliminated the virus. This is called long COVID and can occur even in otherwise healthy people with ‘mild’ cases and even in children. It is important to know this can occur and to speak with your doctor if you are experiencing atypical or persistent symptoms.
- We have seen small numbers of cases of a multisystem inflammatory disease in children that is similar to Kawasaki disease. This disease appears to occur days to weeks after COVID-19 infection in a very small number of children and teenagers. The numbers are very low and overall kids still fare the best of any age group; however, this new disease is very serious and parents should be alert for the possible symptoms. Be on the lookout for the combination of fever and either rash or severe stomach issues (diarrhea, vomiting, or abdominal pain), especially if your child either had COVID-19 or has been exposed to someone that was infected. If you see these symptoms, call your doctor immediately.
- The virus is transmitted through breathing, talking, singing, coughing and through contact with contaminated surfaces (e.g. someone coughs on a door handle, you touch that handle and then touch your mouth).
- There are no cures but multiple treatments have been developed that can somewhat lower the risk of fatalities from severe COVID.
- We also have multiple vaccines that are highly protective and show very good safety profiles.
Prevention:
- Wear a FFP2/FFP2/N95/KN95 or higher quality mask.
- Wash your hands frequently with soap for at least 20 seconds and avoid touching your face (mouth/nose/eyes). If hand washing is not possible, use a disinfectant hand gel (e.g. Purell).
- Regularly clean common surfaces in your house (e.g. door handles, faucet handles, counters) using a disinfectant spray or wipe (e.g. Lysol, Clorox, etc).
- Take care of your health, exercising, eating healthy, ensuring you get enough vitamins and sleep.
- Don’t go to any indoor spaces with others (especially spaces with crowds), don’t have friends over or go to others’ homes.
- Anytime you leave your home, pay attention to washing your hands, not touching your face and keep 6 feet of separation from others. If you can, work from home.
- For a great example of why physical distancing is a great way to stop the spread of COVID-19, please see this New York Times article.
- Do not travel unless necessary.
- Prepare for the possibility of being isolated at home for two weeks if you get sick, making sure you have supplies of food and prescriptions. You don’t need to stockpile, stores will continue to be open!
- Make sure your family understands these precautions, as most cases result from transmission between family members; this is especially important for those at high-risk.
- Pay attention to your health, a slight fever or body ache can be the first sign and the best time to act in order to prevent transmission to others. Isolate, stay at home and call your doctor for advice.
- You do not need to panic or obsess over every small risk. You will never be able to completely eliminate the risk of infection, but though the dedicated practices above you can dramatically reduce your risk. For a good discussion of the precautions, please see this video from a physician working in the center of the initial outbreak in NYC.
- Do not drink, gargle, wash with or inject bleach or isopropyl alcohol, this can be fatal. Also, do not try to use UV light to kill the virus on your body, this is also very harmful. All of these can kill the virus on surfaces (such as a table) but there is no quick easy cure for COVID-19 infections.
- Some hand sanitizers have been found to contain methanol, which can be toxic. Before using a new brand, please check the FDA list of sanitizer brands to avoid.
- For more information, the Biosecurity Research Initiative has created a very detailed discussion of precautions that can be taken in different environments.
What to do if you get sick:
- Stay calm and remember that most cases are very mild. If you just have a runny/stuffy nose without a fever it is likely to be a cold; however, if you have any fever, body aches, coughing or shortness of breath then stay at home and isolate yourself until you have spoken to your doctor.
- Remain at home and call your doctor, they will advise you if you should be tested, where to go and what to do. Do not go directly to the hospital unless you are having trouble breathing.
- Plan on staying at home for two weeks while you recover. If you have to leave the house your doctor may advise wearing a mask to minimize the chances of you infecting others.
- Notify your doctor by phone if your symptoms increase, you have any difficulty breathing or you notice any neurological changes.
- If you are living with others, try to isolate as much as possible (e.g. use separate bed/bathrooms).
- Get any supplies you need delivered to your front door, don’t have anyone come inside.
- Make sure you use tissues when you cough/sneeze, throw them directly in the trash and then wash your hands. Also, regularly clean all the surfaces you touch in the house with disinfectant.
Financial implications of COVID-19:
- Across the world, the uncertainty surrounding the effects of COVID-19 has had rippling financial impacts at both the micro and macro levels.
- At a micro level, individuals may feel the financial impact of COVID-19 in a myriad of ways. From income disruption, to increased spending on food/supplies, to decreases in retirement account value. It is important to recognize the different people will feel the financial impact differently and to know that the financial situation like the spread of COVID-19 is constantly evolving. The importance of remaining calm and practicing good financial habits is amplified during times like this. Specifically, maintain a budget, monitor your spending and be mindful of your debt.
- At a macro level, the general uncertainty, illness, and quarantine (self or otherwise) have impacted all aspects of global and domestic economies by disrupting production, supply chains, financial markets, human capital, etc. It is important to remember that this pandemic is impacting the entire globe and may directly or indirectly impact your financial situation.
The Truth of Some Top COVID-19 Rumors:
When you hear a new story, the old adage holds true, if it sounds too good to be true, it probably is. Remember that anyone can call themselves a doctor, that doesn’t mean they are correct. Confirm any information you hear on social media; does it match with what the WHO or CDC are saying? There are also good guides available online discussing how to spot fake news.
- The disease is the same as the flu. FALSE, it is a respiratory infection and spreads in a similar way, but COVID-19 has a much higher rate of severe infections and a higher case-fatality rate.
- You can get the virus from someone that doesn’t have symptoms. TRUE, research suggests that the virus transmits best at early points in infection when you barely even know you’re infected.
- You can catch it from (or give it to) a pet. MOSTLY FALSE, the virus is thought to originate from wild animals in China, but it is very specific in what it infects. There is a very small chance that pets can be infected, but they do not get sick, do not transmit the virus and no precautions are needed.
- Facemasks will protect you from the virus. PARTIALLY TRUE, certain masks can protect you, but these are specific masks that require proper training. However, the greatest risk of transmission is from touching your face, so if wearing a mask reminds you to not touch your face, this can be useful. You do not need an N95 or surgical mask for this, even a bandana will work. Just remember, it’s only a reminder not to touch your face, it will not protect you from the virus.
- Warm weather will stop the virus. PARTIALLY TRUE, it may slow the virus but not stop it.
- Cold weather will stop the virus. FALSE, most respiratory viruses spread better in cold dry weather.
- Hand dryers will kill the virus. FALSE, hand washing with soap will though.
- Spraying alcohol or bleach on your skin will prevent infection. FALSE, soap and water will safely remove the virus from your skin, spraying bleach or alcohol on your skin is very dangerous.
- Vaccines against pneumonia will protect you against COVID-19. FALSE, the vaccine prevents bacterial pneumonia not viral pneumonia, there is no COVID-19 vaccine.
- Drinking water, gargling or rinsing your nose with saline will prevent the disease. FALSE, there is no evidence to suggest that this will affect the disease or your susceptibility to be infected.
- Drinking hot beverages helps prevent and cold beverages worsens the disease. FALSE, the temperature of liquid you consume has no effect on the COVID-19 disease.
- Antibiotics or antibacterial soap will help fight the disease. FALSE, this is a virus infection and antibiotics or anti-bacterial products will not help, all you need is regular soap and water.
- Hand sanitizers are better than soap. FALSE, soap and water is the most effective and safest way to clean your hands and prevent infection. Hand sanitizers work well, but are harsher to your skin.
- Only older people will get the disease. FALSE, there is a greater risk of severe disease for older people (over 70) but even children can get the disease (though it is typically very mild in children).
- We have medications that will fight the virus or will have a vaccine soon. FALSE, there are some in development but we do not have any approved treatments and a vaccine is months-years away.
- You can self-check for infection by holding your breath without coughing. FALSE, early in infection there are no respiratory symptoms and this ‘test’ does not tell you anything about infection.
- Coronaviruses will survive on metal/fabric/surfaces for several hours. TRUE, COVID-19 can survive on metal or plastic for up to 72 hours and cardboard/paper for 24 hours. Clean your hands with soap and hot water, clean surfaces with a disinfectant cleaner and wash your clothes with laundry detergent and hot water, nothing else is necessary.
- The virus was created in a lab and intentionally spread to damage [fill in your favorite group here]. FALSE, this virus is very similar to SARS and MERS that both naturally emerged, there is no genetic or other evidence to suggest this was intentionally released or designed.
- There’s nothing we can do. FALSE, our surveillance, testing and containment strategies will be effective in time and we can all help by paying attention to the prevention recommendations above.