Big changes, small differences, one constant – the ABCs of COVID
A lot has changed since the world encountered the novel virus commonly known as Coronavirus, and scientifically named SARS-CoV-2, but one thing that hasn’t changed, regardless of which variant is in the news or in what country one is, is how to best prevent the spread of the virus.
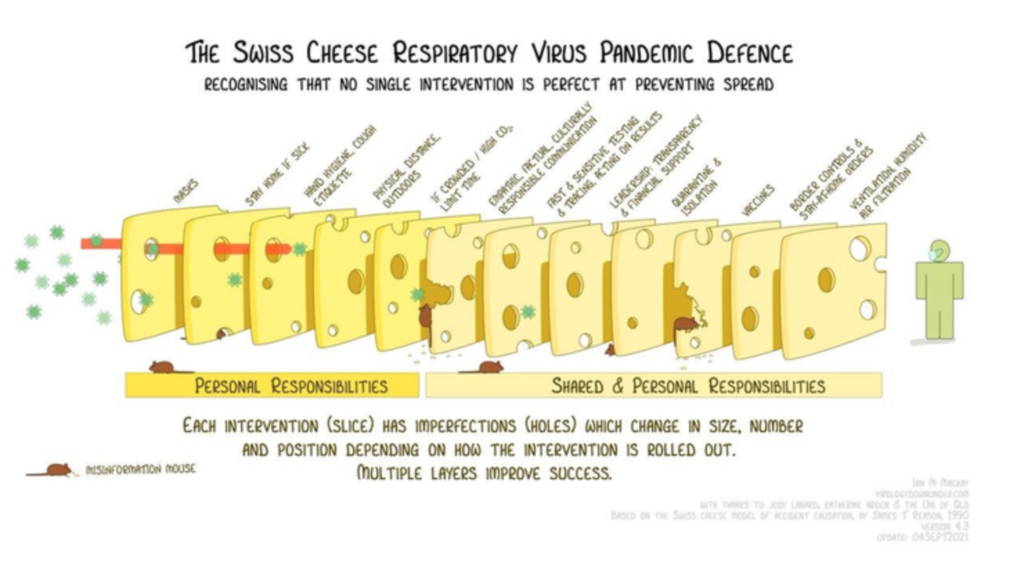
In 2020, a well known and established model used in risk analysis and risk management, the Swiss Cheese model, was adapted by Australian virologist Ian M. Mackay for the coronavirus pandemic. This multi-layer model highlights how no single intervention is perfect at preventing the spread but that a combination of different layers, from nonpharmaceutical interventions (NPIs) to vaccines, at personal and governmental levels is required to break the chain of infection. Vaccines and boosters alone are not enough, a layered mitigation continues to be our best approach.
Goodbye year II, hello to another year of the pandemic ‘How did we get here and why?’
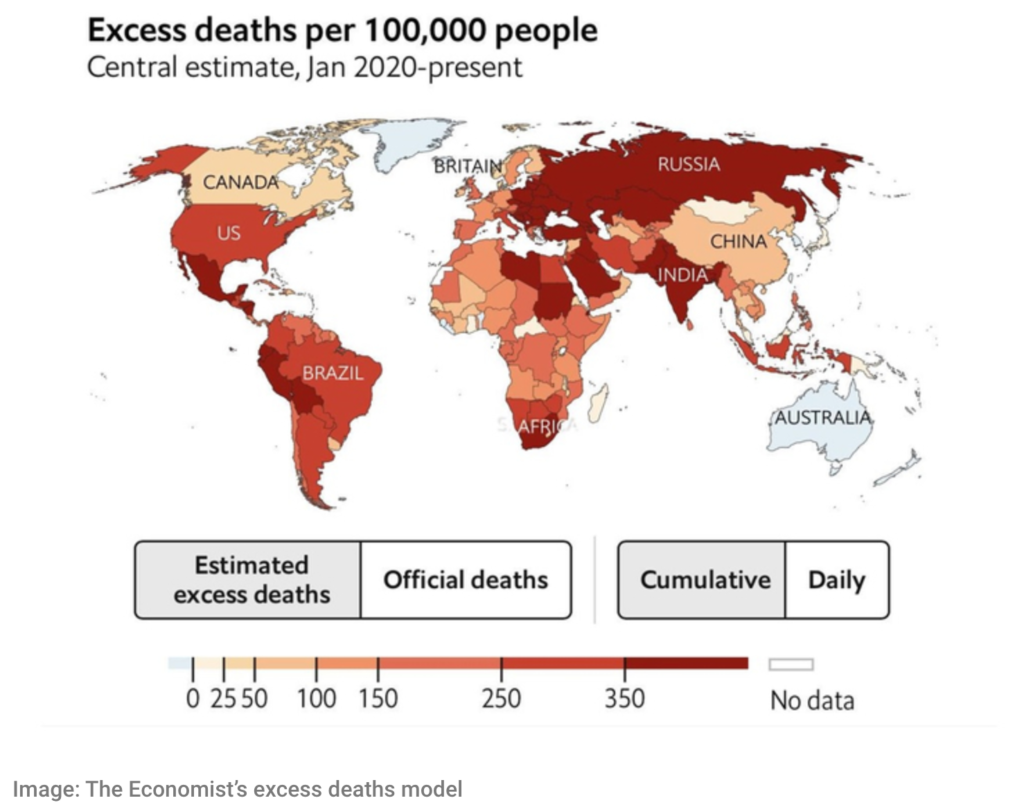
The mortality rate of COVID-19 has been a blessing and a curse for the world. A blessing because, unlike with the Black Plague, people were not dying horrible deaths soon after infection, and a curse because most of the deaths these last two years were underreported –– the true death toll globally, as shown in The Economist’s continuously updated model is 3 times higher than the official toll of 5.4 million –– and not in plain sight, and thus people and countries began, and continue, to minimize the situation.
Lack of sufficient testing and reporting in many countries around the world has made it difficult to accurately know how many people have died. The uncertainty range is quite large, but currently the best estimate is 18.6 million deaths.
Because of this double-edged sword, if there is one thing, since December 2019, that everyone can agree on, it is that great communication and cooperation between entities has been inexplicably absent. A trend with deadly consequences that has been a constant when dealing with this damaging, and for some, deadly virus.
At this stage of the pandemic, with Delta (one of the most worrisome variants of concern) fastly losing its predominant place in the world to the newly identified –– and as of now even more worrisome –– variant of concern Omicron (B.1.1.529) and with vaccines (including the recently required booster shot) being abundant in rich countries but a desperate dream in others, a sharp line needs to be drawn. We need to ask ourselves: “How many more times will we allow ourselves to repeat the same mistakes, our own and others’, before we decide that enough is enough?”
The topic of the year has been, for obvious reasons, the COVID vaccines and the booster shots. From India to Germany, to the UK, to China, to Russia, the US and more, different vaccines were given emergency authorization to be produced and administered in different countries. Weeks and months later, the world had welcomed 2021 with open arms and high expectations –– the vaccines were here, everything would be ok, everything would go back to normal sooner rather than later.
False promises were heard left and right, forgoing once again caution and clarity, stating or insinuating that the pandemic was almost, if not already, over. As summer ended in the northern hemisphere, we unequivocally knew that –– despite what some politicians and media had baselessly reported in Spring 2021, and despite not heeding the early 2021 warnings from Israeland Chile that a vaccine-only strategy was insufficient –– the pandemic is not over.
We are not quite there yet because the usual indispensable duo in a crisis, communication and cooperation, is still missing and because of the strong, stronger than ever, divide between poorer and richer countries in terms of vaccine (in)equity. In countries in Asia, South America, and Africa, people are desperate for a vaccine that they don’t have, while countries in Europe and North America have hoarded vaccines whilst having a slower than required rollout and, because of Omicon, are racing to boost their population as countries reach record high numbers of new daily cases. A Global South without enough vaccines, not even for their health care workers, vs a Global North stubbornly holding onto a vaccine-only strategy as they work on administering booster doses to the double vaccinated and vaccinating children.
Vaccines were often sold to the public as the all encompassing answer –– the solution –– to ending the pandemic. In a moment where hope and improvements were needed, once again, false hope was delivered. We know that the vaccines are very good and are doing what they were meant to achieve –– ensure that if infected the probability of having a severe COVID-19 course, getting hospitalized or dying is substantially lowered. This is extraordinary and gives us hope, something that so many of us need.
But it is not enough.
It is not enough because beyond hospitalization and death there is transmission –– transmission to those not vaccinated and therefore at high risk, and unfortunately also to the vaccinated (though they are at a lower risk of severe disease, they are not completely protected) –– and Long Covid. Add to that, that it is yet not known what percentage of the vaccinated transmit the virus due to Omicron and how much the vaccines lower the chances of developing severe disease with Omicron and reduce the likelihood of developing Long Covid, but estimates make us worry.
It is also not enough because vaccine equity is still not a priority, we see it, for example, in the over 15 million vaccine doses the United States wasted since March 2021 while countries such as Bolivia were left with people calling in every favor owed to find a way to get a vaccine –– any vaccine.
The amount and speed in which vaccines and boosters are, even today, administered is not enough even in the West because maintaining low community transmission has not been a priority in most countries, partly due to some governments not acting on or acknowledging the basics of COVID, and thus not taken into consideration in most countries’ pandemic response, and partly because accountability is not in fashion.
Before the Greek alphabet became part of people’s everyday vocabulary, there already was a variant of concern that was worrisome: B.1.1.7, now known as Alpha. In December 2020, the United Kingdom announced to the world that this new coronavirus variant, first identified in September 2020, was more transmissible and was rapidly spreading. That month, mathematician and epidemiologist Adam Kucharski from the London School of Hygiene & Tropical Medicine, amongst others, went on explaining why a SARS-CoV-2 variant that was more transmissible was a bigger problem than a variant that was 50% more deadly –– another blessing and curse scenario.
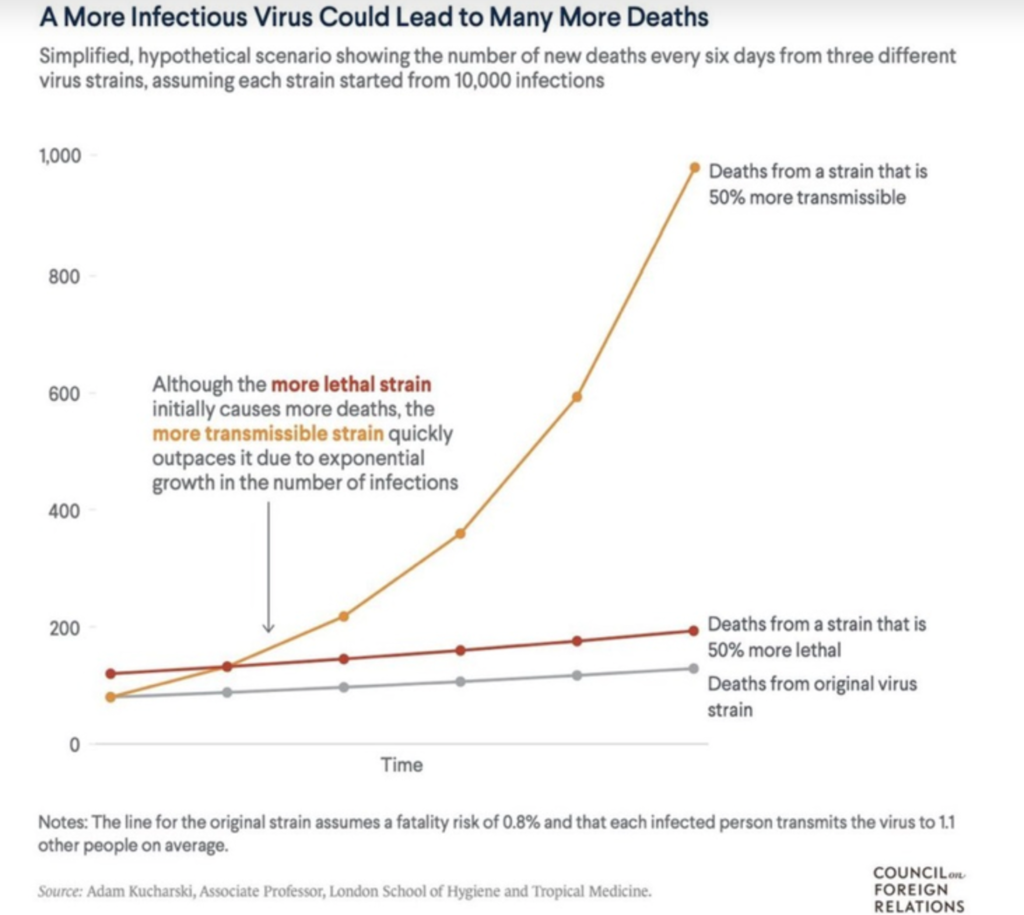
Although a variant which spreads more effectively was exponentially worse for all, few policy makers took this new element into consideration when dealing with the pandemic and so breaking the chain of transmission was still not a priority for most.
Months later, it was predominant in most parts of the world and caused more damage and deaths than the initial strain.
Fast forward to the end of Alpha and the emergence, and the dominance, of Delta, and the importance of transmissibility over lethality remained relevant, after all, Delta was more transmissible, and even more deadly (because of its enhanced transmissibility and possible increases in severity), than Alpha, but once again, policy makers dismissed this difference more often than not.
This dismissal can be seen once again with Omicron. There’s a hope that, although likely more transmissible and much more immune evading than Delta, Omicron will be milder. This assumption and hope, that it is milder, is once again paving the way to another harsh winter and another wave of Long Covid sufferers – mild COVID can cause, and has caused, Long Covid. Even if it is milder, which has not been proven, the enhanced immune evasion and transmission can still lead to significant hospitalization and death, and Long Covid.
We can see the dismissal in every decision, every communication, every action by many governments and media outlets that was based on studies and discussions that predated Alpha and then Delta. This meant that the information shared, and used, on mortality, morbidity, Long Covid, vaccines, restrictions and more, was based on old information that no longer accurately reflected the current situation or there was a selective choosing of which information to share and use. Always two steps behind the virus, always repeating the same mistakes and ignoring best case practices and experiences from countries next door and/or worlds apart.
There are a few certainties in this pandemic that are irrefutable, may it be with Delta or with Omicron, everything else comes down to a mix of circumstances and luck:
● SARS-CoV-2 is a novel virus that causes the disease known as COVID-19
● COVID-19, regardless of the severity of the case, can lead to Long Covid.
● Young and healthy individuals can also go on to develop Long Covid.
● The virus is airborne and any indoor interaction with others –– in a setting with insufficient testing, high community transmission, low fully vaccinated + booster percentage, poor ventilation, lack of mask wearing –– can lead to infection.
● More people infected with the virus means more people getting COVID-19.
● More people with COVID-19 means more people severely sick and more people hospitalized.
● More people with COVID-19 means more people with Long Covid.
● Long Covid can be mild with a few symptoms for a few weeks or months AND Long Covid can be severe, worse off than COVID-19, with 30+ symptoms for a year, two, or more.
● The more the virus circulates, the worse various aspects of our daily life will be affected.
● When community transmission is high and there are little to no epidemic control measures in place (including high vaccination rates), a country is socially, economically, and emotionally worse off.
● The more cases of COVID-19 globally, as we can once again see with the emergence of Omicron, the more chances of a new variant of concern emerging.
Acknowledging how transmission occurs, knowing how it can be prevented, and understanding individual and community risks continue to be our personal tools to protect ourselves and our loved ones. Unfortunately, some or most of the information we receive is still riddled with omissions, half trues, and/or misinformation.
By summer 2020, it was evident (but poorly and insufficiently communicated) that COVID was airborne. And so, even today, over a year later, too many politicians and people are still unaware, or unconcerned, that ensuring good ventilation is one of the most important epidemic control measures we have. For instance, too many schools and workplaces continue to spend money and time on, what has been called, hygiene theater: the cleaning of surfaces and washing hands, which, of course, are very good habits that are good for one’s health, but not what is important and necessary to do when dealing with an airborne virus. Any establishment without proper ventilation, in a town or city where community transmission is high, and where people are close together and without masks is at a higher risk for infection. Working towards the betterment of ventilation in schools, restaurants, offices, and other places is necessary to keep low community transmission.
With this virus, there is no black or white. Instead, there are shades of probabilities based on luck, comprehensive understanding, and economic situation. Where do you live? Do you live in New Zealand or in India or in Germany? Do you live in a small town in the countryside or in a cosmopolitan crowded city? Do you work day to day or have an office job that through technology can be converted into working from home? Do you consider, and/or can you afford to consider, the basics of the virus transmission, such as that the less interactions with people outside of your household the less the likelihood of infecting or getting infected there is, as you live through a pandemic?
This myriad of variables is then added to the overall health of each individual that faces an infection from SARS-CoV-2 and is a reminder that there are no bulletproof categories to ensure an easy experience with the virus, for even a mild course of COVID-19 in a young and healthy person can develop into the debilitating disease of Long Covid. And, as of now, the only certain way to avoid getting Long Covid is by not getting COVID.
There is hope that vaccines will also significantly prevent Long Covid, but it is still too soon to tell by how much and depending on what. To put it in a nutshell, vaccines reduce the chance of getting infected, and so reduce the risk there, but if you do get infected, we don’t know if the vaccines offer much additional protection for Long Covid. In the meantime, the continued creation and spread of misinformation and disinformation is fueled by further confusion and insecurities that have, understandably, enabled vaccine hesitancy and a harmful pandemic fatigue to solidify.
Countries like the US, UK, and Germany have, so far, fully vaccinated only around 60% to 70% of their population. Why are the numbers in these privileged countries not higher? The blame lies on the same culprits: misunderstandings, miscommunication, misinformation, and contradictions. And it is this fatal four that will, sadly and unfortunately, continue to make it overall worse in all countries.
Even with vaccine supply finally available, too many countries’ vaccination numbers, let alone booster numbers, are not as high as the pandemic warrants it –– especially considering that the number of daily cases are as high or higher than a year ago today, that Omicron is likely even more transmissible than what we have experienced thus far, and data so far strongly suggests that vaccines are less effective against this new variant of concern.
Exponential growth of Omicron and a failure to err on the side of caution has ensured that the next few months may be the most difficult yet.
Throughout the pandemic, terms such as pandemic fatigue, calculated risk, and ‘living with the virus’ have made the front page in different languages. At the end of March 2021, governments were citing pandemic fatigue as a reason to loosen restrictions at a time when community transmission with a variant of concern known for being more transmissible and worrisome was high, and at a time when, once again, testing and contact tracing was insufficient and/or inefficient.
Doing less in a pandemic was said to be a calculated risk and for the good of the people.
This did not make sense, for how could this be for the good of the people if the reason why there was pandemic fatigue was not addressed? People were tired of continually taking precautions and having restrictions when there was no confidence this was effective or would lead to any positive change.People were tired because their country’s pandemic response had failed, or was failing, and the words and actions of decision makers were a continuous contradiction to the situation at hand. How could risk be calculated if governments were still not considering Long Covid as an important risk factor? For many, a negative test after COVID did not necessarily mean recovered, it simply meant a negative test for COVID and debilitating long term symptoms.
In addition to Long Covid, how often reinfection occurs is also often overlooked. Not only did studies early this year show that women were less likely to develop antibodies as a result of infection, according to the CDC, 36% of COVID patients never make a robust/protective antibody response (mild and asymptomatic cases, as well as people under 40, are less likely to make antibodies). Knowing this, it is undeniable that increasing the amount of virus circulating in a community increases the likelihood of having Long Covid and reinfections.
Loosening restrictions, at a time when vaccination had only started, was supposed to make things better. Unsurprisingly it didn’t.
We clearly saw it earlier this year when Israel and Chile, soon after they were lauded by the world for their successful vaccination rollout, had one of the worst waves in their countries. Complacency, poor science communication, impatience, and an over reliance on the one measure –– vaccination –– without accounting for the role of transmission, breakthrough infections, Long Covid, etcetera, had backfired. Restrictions were lifted before enough people were fully vaccinated (final dose + 2 weeks) ensuring community transmission to rise faster than the speed of vaccination.
Few months later, in summer, the Netherlands had replicated the same mistake.
In June 2021, Dutch Minister of Health Hugo de Jonge used the play on words Dansen met Janssen to promote vaccination among the young. Those who got their one-shot Johnson & Johnson vaccine were encouraged to go clubbing right after without having to wait for the necessary weeks for the vaccine to generate enough antibodies and without having to get a test. Within weeks, Dancing with Janssen ended in failure and apologies. Fast forward to the weekend before Christmas, and the situation in the Netherlands is dire with the newly –– too little too late –– introduced lockdown.
Once again, today, countries are ignoring what led them to lockdowns, the last resort, and are stumbling and rushing to a normality that in a pandemic can not exist.
A pandemic such as this one is a global health crisis where BAU, the business as usual we were all used to before 2020, can not exist because everything and everyone is affected. Behaving as if the pandemic is over will not make it over.
When countries such as Denmark, Finland, and Sweden, with or without reaching their vaccination rate goals, announced that the pandemic was over in their countries in September/October 2021, or in the UK’s case in July 2021, and that all (or almost all) restrictions would be lifted, they ignored that –– with winter at our doorsteps –– the need to vaccinate more and ensure low community transmission was fundamental. They ignored the lessons learned from countries that have made the same mistakes, and they ignored the population that was not yet vaccinated and the population that could not be vaccinated. We can see this in the families in the UK, and around the world, that have shielded before the pandemic due to one or more family members vulnerable to disease that continue to be overlooked and forgotten.
If we can not be realistic, then, as 2020 and 2021 have tried to teach us, it is better to be pessimistic and prevent, rather than optimistic and regret.
Living in a society where the virus is not controlled, i.e vaccination + getting infections down and keeping them down, continues to be detrimental to people’s lives. As the World Health Organization has tirelessly said since the very beginning, bringing transmission down –– and keeping it down –– is an undeniable necessity.
Vaccination indeed remains one of the most powerful tools we have but that alone is not enough, especially not now with Omicron’s immune evasion and its many unknowns.
Just like a forest fire can not burn forever, this coronavirus pandemic can not be a forever-pandemic. No pandemic lasts forever. Rejoice in that knowledge. Know that there is a beginning, a middle, and an end, and the beginning is over. How we act will define how long the pandemic will last and it will make all the difference when it does.
Our actions will make all the difference in how life will be afterwards.
Article written by Laura Maria Caldarone for Research Aid Networks and Pandemic Aid Networks


